Abstract
Background: Natural Killer (NK) cells are known for their high intrinsic cytotoxic capacity. Recently, we and others showed that virally transduced NK cells equipped with a synthetic chimeric antigen receptor (CAR) targeting CD19 induced enhanced killing of acute lymphoblastic leukemia (ALL) cells. Here, we demonstrate for the first time that primary NK cells can be engineered using the non-viral Sleeping Beauty (SB) transposon/transposase system to stably express a CD19-CAR with a safe genomic integration profile and high anti-leukemic efficiency in vitro and in vivo.
Methods: Primary NK cells were isolated from PBMCs from healthy donors. SB transposons vectorized as minicircles (MC), which encode either a Venus fluorescent protein or a CD19-CAR together with truncated EGFR (tEGFR) as a marker, were introduced in combination with the hyperactive SB100X transposase into primary NK cells via nucleofection. The genetically engineered NK cells were expanded using IL-15 cytokine stimulation under feeder-cell free conditions. Vector integration sites were mapped by analyzing the genomic region around each insertion site in genomic DNA from long-term cultivated gene-modified NK cells, engineered ether by lentiviral (LV) or SB-based technology. Stable gene delivery and biological activity were monitored by flow cytometry and cytotoxicity of CD19-CAR NK cells against CD19-positive ALL and CD19-negative cell lines.
Results:
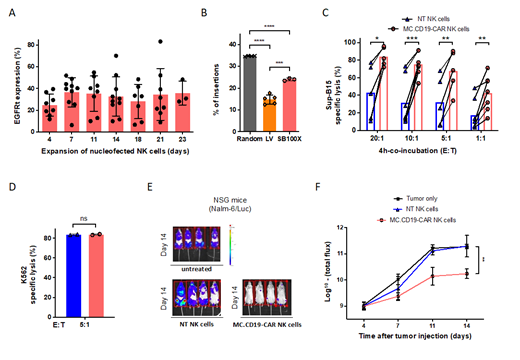
Applying a protocol optimized with respect to nucleofection pulses, time points and plasmid ratios, primary NK cells showed long-lasting Venus expression (up to 50%) upon SB-mediated gene delivery with similar viability as non-treated (NT) NK cells during feeder-cell free ex-vivo expansion using IL-15. Likewise, SB transposon-engineered CD19-CAR NK cells displayed high viability, durable transgene expression (Fig 1 A), and no significant change in the NK cell phenotype profile.
Next, we assessed vector integration into genomic safe harbors (GSH). GSH are defined as regions of human chromosomes that fulfill the following five criteria: not ultraconserved, >300 kb away from miRNA genes, >50 kb away from transcriptional start sites (TSS), >300 kb away from genes involved in cancer and outside transcription units. CD19-CAR NK cells generated using SB100X showed a significantly higher frequency of vector integration into GSH compared to LV-transduced CAR-NK cells and a significantly more-close to random nucleotide frequency (computer-generated random positions in the genome map to GSHs; random 43.68%; LV 14.78%, SB100X 23.99%; p<0.05) (Fig 1 B).
MC.CD19-CAR NK cells generated with the SB platform demonstrated significantly higher cytotoxicity compared to NT NK cells against CD19-positive Sup-B15 ALL cells after long-term cultivation for two to three weeks and no loss of natural intrinsic cytotoxicity. After 4-hour co-culture, significantly enhanced specific tumor cell lysis was found for MC.CD19-CAR NK cells vs NT NK cells at all effector to target cell ratios (E:T) tested (E:T 20:1 83.88% vs 43.13%; E:T 10:1 75.18% vs 31.32%; E:T 5:1 67.38 vs 32.22%; E:T 1:1 42.54 vs 10.19%; p<0.05) (Fig 1 C). With regard to intrinsic natural cytotoxicity of NK cells, no significant decrease in cell killing was overserved for SB-gene-modified CD19-CAR NK cells compared to NT NK cells against CD19-negative K562 cells (E:T 5:1 83%; p<0.05) (Fig 1 D).
Significantly enhanced antitumor potential of SB-generated CD19-CAR NK cells was confirmed in a systemic CD19-positive lymphoma xenograft model (NSG-Nalm-6/Luc) in vivo. After injection of 0.5x10 6 tumor cells per mouse and lymphoma engraftment, animals were treated with a single dose of 10x10 6 SB-modified CD19-CAR NK cells pooled from three different donors with a mean tEGFR/CAR expression of 34%. MC.CD19-CAR NK cell therapy resulted in rapid lymphoma eradication in all treated mice (n=4; p<0.05), whereas mice receiving similar amounts of NT NK cells showed progressive lymphoma growth comparable to untreated control mice (Fig 1 E-F).
Conclusion: Taken together, the Sleeping Beauty transposon system represents an innovative gene therapy approach for non-viral engineering of safe, highly functional and relatively cost-efficient CAR-NK cells that may not only be suitable for ALL therapy but also for a broad range of other applications in cancer therapy.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal